Exploring the Science of Recovery

Originally published in the winter 2017 issue of the American Fitness Magazine.
Recovery from training is becoming recognized as one of the most important aspects of physical activity and overall wellness. As we sort through the myriad recovery strategies and their varied levels of scientific support, it’s important to remember that both scientific and anecdotal evidence point to the value of an appropriate recovery plan to encourage adaptation, wellness and performance.
Although some may prove more effective than others, it’s crucial to remember that any interventions will likely work better when tailored to individual clients. Keep in mind that the most effective strategy for you might be to experiment to determine which ones prove feasible and successful for the people you work with.
Understanding Recovery
We eat, sleep, train, repeat—constantly striving to get bigger, stronger, faster or slimmer—but is there a point where too much becomes harmful? Many recognize the need for recovery after exercise, but do we understand what it takes to fully recover and whether we have actually achieved that state? We hear terms like overtraining and nonfunctional overreaching (the threshold just prior to overtraining) and wonder “Why do they get so much attention today?”
Answering these questions starts with a basic understanding of homeostasis, stress and recovery within the body.
- Homeostasis is a state of balance within the body that occurs when the variables in a system (e.g., pH, temperature) are regulated to keep internal conditions stable and relatively constant (Pocari et al. 2015).
- Stress is a stimulus that overcomes (or threatens to overcome) the body’s ability to maintain homeostasis. In this article, we will focus on stress related to exercise, which includes physiological (e.g., muscle tears, dehydration, pain) and chemical (e.g., blood imbalances of acid-base or oxygen-carbon dioxide). Other common types of stress are environmental (e.g., cold, humidity), psychological (e.g., finances), emotional (e.g., fear, anxiety) and social (e.g., interpersonal conflicts).
- Recovery is the body’s process for restoring homeostasis.
The human body is designed to tackle stress—we either adapt or perish (hence the concept of “survival of the fittest”).
An intense, acute bout of physiological stress followed by adequate recovery, which enables adaptation and restores homeostasis, is generally considered healthy (Sapolsky 2004). However, physiological stress that is not followed by adequate recovery can, over time, compromise homeostasis and immune function, increasing the probability of injury, illness and the onset of nonfunctional overreaching or overtraining. Considering these implications, it’s no surprise that experts have turned their attention to studying stress and recovery.
Types of Recovery
Though recovery is a critical phase of the exercise-adaptation cycle, it is among the least understood and most under-researched components of training. Essentially, recovery is a process that includes rest, refueling, rehydration, regeneration (repair), resynthesis, reduction of inflammation and restoration that ultimately returns the body to homeostasis.
Jonathan Ross, a highly recognized and respected trainer from Baltimore, advises his clients that if they’re “hitting it hard,” then they need to devote equal time to “quitting it hard” to appropriately recover.
It’s helpful to think of three categories of recovery:
- Immediate recovery, which happens in the short time between successive efforts, e.g., between repetitions within a set of biceps curls
- Short-term recovery, which happens between sets, e.g., between interval sprints or weight training sets
- Training recovery, which happens between workouts or competitions (Bishop et al. 2008)
Focusing on training recovery offers the greatest potential benefit because everything that happens outside of an exercise session—i.e., life—has a potential impact. Hence, the need to ask: Are we truly recovering from training, given the body’s perception of stress and the hectic schedules many of us keep? Furthermore, how do we measure or monitor recovery?
Monitoring Recovery
Usually, an evening of restful sleep coupled with good nutrition and hydration will restore homeostasis and full recovery (Pocari et al. 2015). However, we can now monitor various physiological parameters in real time to validate recovery and improve the recovery process.
For example, measuring resting heart rate (RHR), heart rate variability (HRV) and ventilation (breathing) patterns can provide valuable information on the dominance of our sympathetic nervous system (SNS) or parasympathetic nervous system (PNS), the latter of which is responsible for rest, repair and recovery. It’s also helpful to review the scientific evidence for six specific means of achieving it: active recovery, massage, compression, cryotherapy, hydrotherapy and sleep.
Active Recovery
Two studies highlight the value of active recovery, which typically uses movements ranging from spurts of anaerobic activity to very light-intensity activity (e.g., cool down). The idea is to accelerate the removal of lactate and hydrogen from muscles while stimulating blood flow and signaling proteins (to initiate healing/adaptation) into the localized tissue.
One study found that active recovery after repeated intense exercise resulted in faster returns to homeostasis compared with passive recoveries that used no movement (Ahmaidi et al. 1996). Another study found that following high-intensity work with active recoveries performed at 60–100% of lactate threshold helped muscles recover faster than did more passive recoveries performed at lower intensities at 0–40% of lactate threshold (Menzies et al. 2010).

Massage
Advocates of massage say it decreases muscle soreness, pain and stress, improves circulation and lymphatic flow, and creates an enhanced perception of recovery. Researchers, however, have questioned its value and warn of its potential to create more muscle damage if performed too aggressively or too soon after exercise (Schaser et al. 2007; Wiltshire et al. 2010).
One study discovered that massage performed immediately after exercise resulted in reduced blood flow and impaired removal of lactate and hydrogen ions from muscles, thereby slowing recovery (Wiltshire et al. 2010). By contrast, other researchers discovered increased muscle activation and proprioception, and reductions in delayed onset of muscle soreness (DOMS) with massage (Shin & Sung 2014).
In yet another study that examined cycling performances separated by 24 hours, massages were found to be superior to passive recovery, but a combination of active recovery and cold-water immersion provided slightly greater benefits than massage (Lane & Wenger 2004). Despite massage’s popularity, few reports demonstrate positive effects on repeated exercise performance. Consequently, we still cannot say if massages are truly effective at influencing muscle and overall recovery.
Compression
Delivered via clothing or through inflatable devices (e.g., pulsatile pneumatics), compression is believed to alleviate muscle fatigue and soreness, accelerate lactate and metabolic byproduct removal, reduce muscle stiffness, increase venous and lymphatic flow and muscle oxygenation, and accelerate recovery while also improving performance.
Various studies examining the effects of elastic compression (i.e., fabrics) and pneumatic compression (e.g., prosthetics) have generally concluded that both benefits and drawbacks do exist, but without any risk of harm (O’Donnell et al. 1979; Miyamoto et al. 2011; Cochrane et al. 2013).
Elastic compression clothing (which incorporates constant pressure) appears to reduce some muscle soreness and perception of fatigue, but it also slows the removal of metabolic byproducts. Pneumatic compression (which incorporates pulsatile pressure) tends to have a greater effect on increasing blood flow and decreasing muscle stiffness, but it offers little or no improvement in power, strength or performance.
Miyamoto et al. examined markers of muscle damage (e.g., creatine kinase, interleukin-6) and found no clear evidence of attenuation of these markers with compression that would indicate accelerated rates of recovery (Miyamoto et al. 2011). Although research is somewhat minimal on the true effects of compression, there appear to be some small recovery benefits with little concern about harmful side effects (Hill et al. 2014).

Cryotherapy
Cryotherapy temporarily reduces muscle temperature, stimulating vasoconstriction and reducing inflammation and pain. Critics of cryotherapy point to an overall slowing of normal regenerative inflammation and an increasing risk of further injury from extended exposure of skin and nerves to cold temperatures (Schaser et al. 2007). Some practitioners now advocate alternating hot and cold applications, but little research supports this practice.
Although post-exercise cryotherapy remains popular, the reality is that temporary muscle cooling is unlikely to have a significant influence on muscle repair or recovery. Furthermore, in animal-based studies, it did delay recovery (Schaser et al. 2007). Unfortunately, the evidence on cryotherapy’s usefulness is weak and inconclusive due to research inconsistencies involving study design, temperature and duration.

Hydrotherapy
The cardiovascular system responds to hydrotherapy (water immersion) by changing heart rate, peripheral blood flow and resistance to flow. It also changes the temperature of the skin, muscles and core, influencing inflammation, immune function, muscle soreness and perception of fatigue. The three most common immersion techniques are cold water immersion (CWI), hot water immersion (HWI) and contrast water therapy (CWT), which alternates immersions between hot and cold water.
These techniques have been extensively examined and appear to have some benefit, although CWI and CWT demonstrate greater benefits than HWI (Halson 2013). In one study, CWI treatment demonstrated lower perceptions of muscle soreness and smaller decrements in muscle strength 24 and 48 hours post-exercise versus CWT (Ingram et al. 2009).
Sleep
The fields of health and medicine recognize the importance of sleep upon overall health and wellness. Sleep and recovery depend on two vital data points:
- Basal sleep, which is the amount the body needs every night to recover
- Sleep debt, which accumulates if we do not get our basal sleep every night
If sleep debt piles up, rising stress and cortisol accumulation in the body will impair recovery and threaten our health. Considering how much psycho-emotional stress people deal with every day, trainers should take time to inventory the stress their clients or athletes face outside of their workouts and consider the ramifications on recovery and performance. Disregarding or underestimating the importance of sleep may expose your clients to a higher risk of nonfunctional overreaching or overtraining.
The Signs of Overtraining
Hans Seyle, the pioneering stress researcher, wrote that the “exhaustion phase” of his General Adaptation Syndrome increases the risk of injury or illness (Seyle 1978). That phase is synonymous with overtraining.
Though several signals point to overtraining, an elevated resting heart rate (RHR) coupled with a decrease in exercise performance over 7–10 days are perhaps the easiest to monitor (Pocari et al. 2015; NASM 2107).
By contrast, strength recovery is a consistent and effective marker of muscle recovery. Although objective markers of muscle recovery like creatine kinase (CK) are considered valid, the utility of CK is reduced by several variables including gender, age and individual biological responses.
Symptoms of overtraining include:
- Decreased performance over 7–10 day period
- Increased resting heart rate and/or blood pressure
- Decreased body weight
- Reduced appetite or loss of appetite and possibly some nausea
- Disturbed sleep patterns and inability to attain restful sleep
- Muscle soreness and general irritability
- Reduced motivation/adherence
If a client or athlete has symptoms of overtraining, you’ll want to identify the causes and suggest solutions. As Figure 1 shows, solutions may include deloading (reducing training load and/or volume), offloading (ceasing exercise temporarily) or redirecting (changing activity) for a brief period (e.g., a few days to 1–2 weeks) or until the symptoms subside.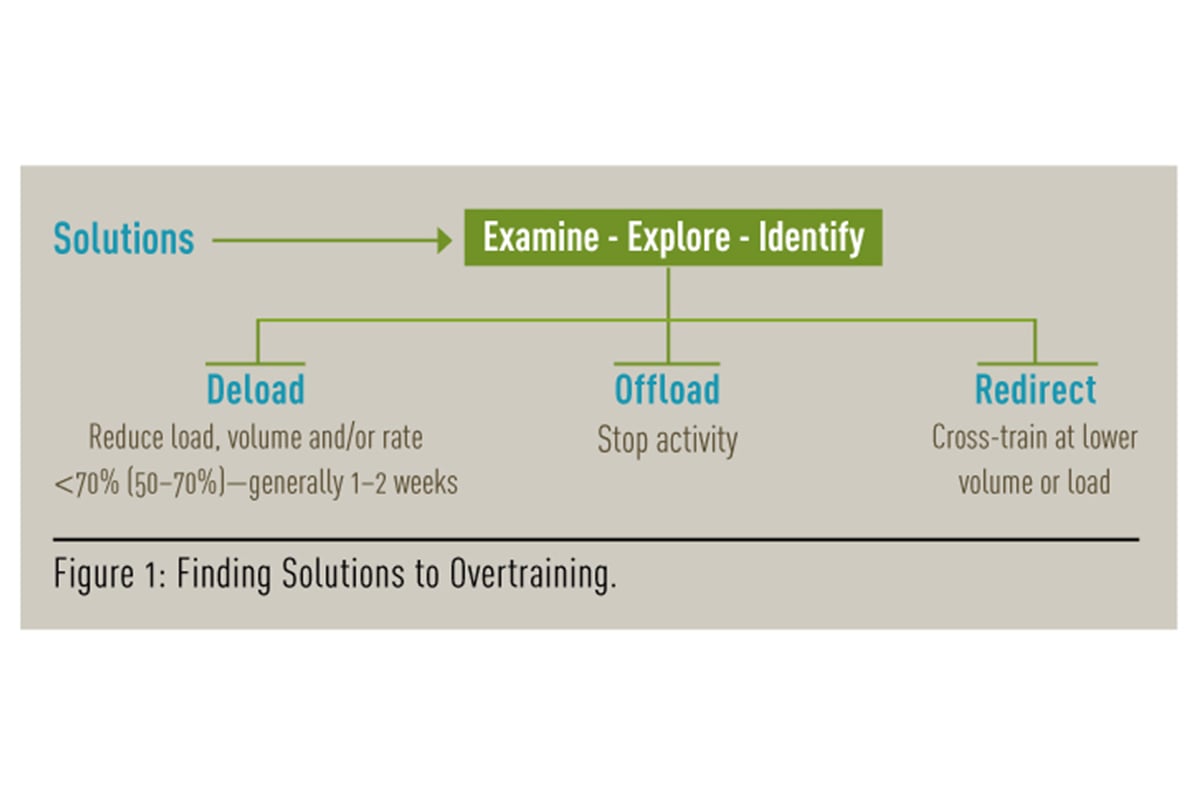
From RICE to CAM
It is interesting to note a small paradigm shift in the suggested protocols following injury and exercise, with some practitioners moving
away from the traditional RICE practice (rest, ice, compress, elevate) and toward CAM (compression, activity, massage).
Pete McCall, a highly respected trainer and fitness educator, is one such practitioner who strongly advocates the use of compression techniques during recovery.

Monitoring Breathing
A person’s depth and rate of breathing (ventilation) both undergo significant changes under stress. At rest, dominance of the parasympathetic nervous system results in slower and relatively deeper breathing (which is preferable), whereas dominance of the sympathetic nervous system results in more rapid and shallow breathing moving toward hyperventilation. Teaching your clients to be more aware of their breathing patterns is an inexpensive and effective way to assess their stress recovery.
One simple method is the Buteyko Control Pause (CP) test, created by a Ukrainian doctor named Konstantin Pavlovich Buteyko to determine whether people are overbreathing. Overbreathing forces greater amounts of carbon dioxide out from the lungs, resulting in a decrease in available bicarbonate in the blood and potentially decreasing one’s capacity for high-intensity exercise.
Buteyko’s test measures the elapsed time between the end of one normal expiration and the point at which the person needs to take another normal breath. The natural delay between breaths is called the automatic pause. Longer pauses are associated with slower, deeper breaths that oxygenate more effectively (because more air is reaching the alveoli), as well as stabilization of blood levels of carbon dioxide, which is important for maintaining blood pH. All of this plays significantly into exercise and recovery.
To conduct Buteyko’s CP test:
- Perform the test in the morning after waking and while sitting upright.
- At end of one normal breath (exhalation), start a stopwatch.
- Sit quietly until the need to take another normal breath occurs. (This cannot be a deeper breath or gasp.) Stop stopwatch.
- The point at which another normal breath is needed should occur at approximately 40 seconds, though many people tend to overbreathe, resulting in a score of only 15–25 seconds.
Monitoring Heart Rate
Monitoring Resting Heart Rate (RHR) can be done simply by having the client take his pulse manually or by using a wrist device or heart rate monitor. You can determine a client’s RHR by averaging several of his heart rate measurements over a 5-day period, taken when the client wakes in the morning (NASM 2017).
In the fitness setting, the client’s heart rate should be no more than 8 beats per minute higher than his RHR. If the client’s heart rate is higher than that, “it is advised that the client take that day off from training.”
Heart rate variability (HRV) is a physiological phenomenon that reflects the time variation (interval) between successive heartbeats. When our parasympathetic nervous system (PNS) dominates, heart rate (HR) varies; it accelerates during inspiration and decelerates during expiration (a healthy sign). By contrast, when our sympathetic nervous system (SNS) dominates, HR shows little variability during breathing (an unhealthy sign).
After we wake from sleep, the body should demonstrate good HRV, which is evidence of PNS dominance, recovery and good health.
HRV is by no means new, as it has been used to predict myocardial infarction risk and other heart-health measures (e.g., diabetes) in medicine for over 40 years.

The Future of Recovery
Technology to measure and encourage recovery is under development. For example, we’ll soon be able to buy tracking devices for the central nervous system that show whether the sympathetic or parasympathetic system is dominant. Disposable or reusable cortisol-monitoring patches also are on the way.
And a new assortment of strain gauges embedded within the fabric of shirts is already able to detect breathing rate, depth, ventilatory power and rate of chest dimension change—though these products are currently too expensive for much of the fitness community. In the future, when prices descend, their data may help everyday exercisers determine where they are on the stress-recovery continuum.
In addition, current research at the cellular level may one day be applied to the field of exercise recovery. For example, Japanese researcher and Nobel Prize winner Yoshinori Ohsumi has spent his career studying a concept of cellular recycling called autophagy, which explains how cellular components are degraded and recycled for use as fuel and building blocks.
Although Ohsumi’s current studies focus on finding medical treatments for disease, the notion of using his findings to expedite recovery after exercise-induced cellular damage is not farfetched.
REFERENCES:
Ahmaidi, S., et al. 1996. Effects of active recovery on plasma lactate and anaerobic power following repeated intensive exercise. Medicine and Science in Sports and Exercise, 28 (4), 450–456.
Bishop, P.A., Jones, E., & Woods, A.K. 2008. Recovery from training: a brief review. Journal of Strength and Conditioning Research, 22 (3), 1015–1024.
Cochrane, D.J., et al. 2013. Does intermittent pneumatic leg compression enhance muscle recovery after strenuous eccentric exercise? International Journal of Sports Medicine, 34 (11), 969–974.
Halson, S.L. 2013. SSE #120: Recovery Techniques for Athletes. Gatorade Sports Science Institute. Accessed Oct 24, 2016: www.gssiweb.org/Article/sse-120-recovery-techniques-for-athletes.
Hill, J., et al. 2014. Compression garments and recovery from exercise-induced muscle damage: a meta-analysis. British Journal of Sports Medicine, 48 (18), 1340–1346.
Ingram, J., et al. 2009. Effect of water immersion methods on post-exercise recovery from simulated team sport exercise. Journal of Science and Medicine in Sport, 12 (3), 417–421.
Lane, K.N., & Wenger, H.A. 2004. Effect of selected recovery conditions on performance of repeated bouts of intermittent cycling separated by 24 hours. Journal of Strength and Conditioning Research, 18 (4), 855–860.
Menzies, P., et al. 2010. Blood lactate clearance during active recovery after an intense running bout depends on the intensity of the active recovery. Journal of Sports Science, 28 (9), 975–982.
Miyamoto, N., et al. 2011. Effect of pressure intensity of graduated elastic compression stocking on muscle fatigue following calf-raise exercise. Journal of Electromyographical Kinesiology, 21 (2), 249–254.
NASM (National Association of Sports Medicine). 2017. McGill, E.A., & Montel, I.N. (editors). NASM Essentials of Personal Fitness Training (5th ed). Burlington, MA: Jones and Barlett Learning.
O’Donnell, T.F., et al. 1979. Effect of elastic compression on venous hemodynamics in postphlebitic limbs. Journal of the American Medical Association, 242 (25), 2766–2768.
Pocari, J.P., Bryant, C.X., & and Comana, F., 2015. Exercise Physiology. Philadelphia: F.A. Davis.
Sapolsky, R.M. 2004. Why Zebras Don’t Get Ulcers (3rd ed). New York: Holt Paperbacks.
Schaser, K.D., et al. 2007. Prolonged superficial local cryotherapy attenuates microcirculatory impairment, regional inflammation, and muscle necrosis after closed soft tissue injury in rats. American Journal of Sports Medicine, 35 (1), 93–102.
Seyle, H. 1978. The Stress of Life New York, NY: McGraw-Hill.
Shin, M.S., & Sung, Y.H. 2014. Effects of Massage on Muscular Strength and Proprioception After Exercise-Induced Muscle Damage. Journal of Strength and Conditioning Research, 29 (8), 2255–2260.
Wiltshire, E.V., Poitras, V., & Pak, M. 2010. Massage impairs post-exercise muscle blood flow and “lactic acid” removal. Medicine & Science in Sports & Exercise, 42 (6),1062–1071.